Classification and incidence of adverse events
It’s important to recognise, respond to and report suspected adverse events.
Once you suspect an adverse reaction, follow the steps for managing suspected transfusion reactions.
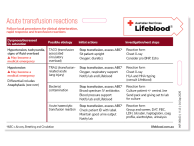
Classification of transfusion-related adverse reactions and estimated incidence
- Immunological acute (<24 hours)
Adverse event Incidence* Acute haemolytic transfusion reaction (AHTR) 1:76,000 Fatal acute haemolytic reaction 1:1.8 million Febrile non-haemolytic transfusion reaction (FNHTR) 0.1%–1%
(with universal leucocyte depletion)
Mild allergic reactions (urticarial/pruritis) 1%–3% of plasma containing components Severe allergic reactions (anaphylaxis) 1:20,000–1:50,000 Transfusion-related acute lung injury (TRALI) 1:1,200–1:190,000 Transfusion-associated dyspnoea 0.4%–3.4% - Non-immunological acute (<24 hours)
Adverse event Incidence* Complications of massive transfusion Variable Non-immune mediated haemolysis (physical or chemical destruction of blood) Rare Transfusion transmitted bacterial infection (for clinically apparent reactions) due to platelets Approximately 1:250,000
(in Australia)**
Transfusion transmitted bacterial infection (for clinically apparent reactions) due to red cells Approximately 1:2.5 million
(in Australia)**
Transfusion-associated circulatory overload (TACO) 1–2.7% - Immunological delayed (>24hours)
Adverse event Incidence* Delayed haemolytic transfusion reaction (DHTR) 1:500–1:10,000 Post-transfusion purpura (PTP) Rare Transfusion-associated graft versus host disease (TA-GVHD) Rare Alloimmunisation - RBC antigens 1% Alloimmunisation - HLA antigens 10% Transfusion-related immune modulation (TRIM) Not known - Non-immunological delayed (>24hours)
Adverse event Incidence* Iron overload Increased morbidity and mortality associated with cumulative doses of 20 or more units Transfusion-transmissible infections For incidence refer to risk estimates for transfusion-transmissible infections
* May be based on overseas data.
** Based on Lifeblood data.
Updated August 2025