Administration
Transfusion of blood components should only be undertaken where appropriate staff and facilities are available to identify and manage any potential adverse transfusion reactions.
Overnight or out of hours transfusions should be avoided unless clinically indicated by the patient’s condition.
The following is only a guide for the administration of blood components, individual hospital guidelines and procedures should be followed.
- Pretransfusion preparation essentials
Ensure the following are in place before transfusion:
- Staff and equipment are available, and transfusion is occurring in a safe clinical area.
- Resuscitation equipment is available, in working order, and emergency medical support is readily available.
- All transfusion equipment is:
- approved for its intended use in blood component transfusion
- in date, has been checked
- used following the manufacturer’s recommendations and specifications
- used in keeping with local health service policy.
- Informed consent discussion has occurred and has been documented.
- Blood transfusions must have a valid informed consent.
- It can be provided by the patient, parent or legal guardian, or follow the emergency medical procedure consent protocols.
- Consent must be documented in the patient’s medical record and/or on a transfusion-specific consent form in accordance with local health service policy.
- Refer to your local health service policy regarding consent processes for blood transfusion, including inability to obtain consent and for patients who refuse.
- All elements of the consent process should be aligned to local, state or territory and national requirements.
- Prescription is complete and valid.
- The treating physician is responsible for completing the prescription and documenting any special requirements.
- IV access is patent and appropriate to use.
- If uncertain, consult with your senior nurse or medical officer.
- Correct patient ID band is attached to the patient.
- Ask the patient (if conscious and competent) to state and spell their first and family names in full, state their date of birth (DOB), and ensure the stated information is identical on the identification band.
- The patient understands the procedure and possible adverse events.
- The person administering the component should ensure the patient understands the transfusion procedure, including symptoms of possible transfusion reactions.
- Record baseline observations.
- Within the 60 minutes before commencement of each pack, record patient temperature, pulse, respirations, blood pressure and general patient status, including any pre-existing rashes.
- Administer premedication if ordered.
- If any premedication has been ordered, ensure it has been administered at the appropriate time prior to commencing transfusion.
Equipment
- Administration sets
- Use of blood administration sets:
- Blood components must be transfused using an administration set approved for this purpose. The set must incorporate a filter (170 to 200 µm) that removes clots and small clumps of debris that may form during collection and storage.
- Platelets must be transfused through a new blood administration set unless administered in the setting of massive or rapid transfusion, in which case platelets and plasma may need to be transfused through the same administration set.
- Platelets must not be transfused through a blood administration set that has been used for red cells, because red cell debris may trap infused platelets. Red cells may follow platelets through the same blood administration set, but not precede platelets.
- Albumin and IV immunoglobulin formulations that do not require reconstitution may be administered via either a standard IV administration set without a filter, or a blood administration set.
- For other plasma-derived blood products, individual product information should be consulted.
- Bedside leucocyte filters are not required in Australia as platelets and red cells provided by Lifeblood are leucocyte depleted.
- Priming and flushing blood administration sets:
- The blood administration set may be primed with the blood component or 0.9% sodium chloride.
- Flushing blood administration sets with a small amount of 0.9% sodium chloride between red cell packs is not evidence-based and may be unnecessary. However, 0.9% sodium chloride may be required to maintain IV access if the next red cell unit is not readily available.
- Changing blood administration sets:
- The blood administration set must be changed when the transfusion is completed, or every 12 hours if the transfusion episode is not yet complete.
- Any number of red cell units may be transfused during a 12-hour period, provided the flow rate remains adequate and manufacturer’s recommendations are not exceeded.
- A new blood administration set should be used if infusions of another fluid, medication or platelets is to continue after the current transfusion (see above).
- Use of blood administration sets:
- Infusion devices and blood warmers
- Use of all equipment to administer blood components including volumetric infusion and external pressure or rapid infusion devices, syringe drivers and blood warmers, should follow local health service policy.
- Equipment must undergo constant monitoring, calibration and maintenance.
- Local health service policy should indicate whether volumetric infusion and external pressure or rapid infusion devices and blood warmers can be used, including in which clinical situations they are appropriate.
- Devices must be validated by the manufacturer for the administration of blood products and used exactly as specified by the manufacturer.
- Concurrent fluids and medications
- IV fluid solutions must not be co-administered with blood components unless there are sufficient data to ensure compatibility.
- Refer to local health service procedures and ANZSBT guidelines for detailed guidance on concurrent fluids and medications.
Compatible fluids:
- The only IV fluid universally compatible with blood components is 0.9% sodium chloride. Red cells are compatible with ABO-compatible plasma and albumin.
- For fluids compatible with plasma-derived and recombinant products refer to the individual product information.
Incompatible fluids:
- Certain IV fluids are incompatible with blood components; for example:
- Electrolyte and colloid solutions containing calcium (such as Haemaccel®, Hartmann's solution, lactated Ringer's solution) must never be added to, or administered through the same IV line as blood components containing citrated anticoagulant because they may cause clotting of the infusion line.
- 5% dextrose in water or hypotonic sodium solutions may cause red cells to haemolyse.
Medications:
- Medication must not be added to the blood bag or blood administration set or IV line before or during transfusion.
- Additional IV access should be obtained in the absence of a multi-lumen CVAD, and when medications or fluids require administration without interruption of concurrently transfused blood products.
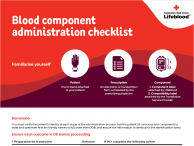
Pre-administration check of the patient, prescription and pack
The final pre-administration check is a vital step of the transfusion process and the last chance to ensure the right component is transfused to the right patient.
- Each individual undertaking the administration of blood components should have an understanding of their roles and responsibilities.
- Two staff members must independently perform uninterrupted checks at the patient’s side immediately prior to transfusion.
- If there is any interruption or a delay, the checking process must be repeated.
- Prior to administration, both clinicians must compare, confirm and be individually satisfied that this is the right pack for the right patient.
- One of the two people involved in the checking process must spike and hang the blood component immediately after checking.
Required checks
- Patient identification
All patients receiving a blood product whether inpatient, outpatient or day patient, must be positively identified.
- Where possible, involve the patient in the identification checks by asking them to state and spell their first and family names in full, state their DOB, and ensure that the stated information is identical on their identification band.
- If the patient is not able to participate, ask a parent, guardian or carer (if present and able) to verify the patient’s identity.
- If the patient’s identity cannot be confirmed, follow local health service policy.
- For the purpose of checking identity, sometimes neonates are known as ‘baby of’ until they have been given a legal name. In the event that the neonatal patient’s identification details change, a new identification band must be attached to the patient.
- Pack integrity
Ensure the pack and component is suitable for transfusion:
- within expiry date and time
- no visible leaks at ports and seams
- no evidence of haemolysis, unusual discolouration or cloudiness, and
- no visible clots.
- Patient and compatibility label
Make sure the patient’s identification band details are identical to the information on the compatibility label attached to the pack. These include:
- patient first and family name, including spelling
- patient DOB, and
- patient medical record number (if unavailable, check local policy for approved 3rd identifier).
- Compatibility and component labels
Compare the compatibility label attached to pack with the Lifeblood component label attached to the pack:
- donation identification numbers are identical, and
- ABO blood group is compatible.
Ensure the blood component has not passed its crossmatch expiry date and time.
- Patient and prescription
Compare all patient identifiers and ensure they are identical on the identification band and prescription, including:
- patient first and family name, including spelling
- patient DOB, and
- patient medical record number.
- Prescription and pack labels
Compare all patient identifiers and ensure they are identical on prescription and compatibility label including:
- patient first and family name, including spelling
- patient DOB, and
- patient medical record number (if unavailable, check local policy for approved 3rd identifier)
Compare the blood component type and ensure it is the same as that on the prescription.
Ensure that any special requirements have been met.
- Administration of blood components
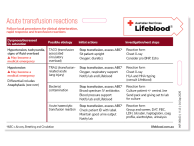
- Frequent visual observation of the patient before, during and after the transfusion is essential to identify possible adverse reactions.
- If an adverse transfusion reaction occurs, stop the transfusion immediately, activate emergency care / rapid response if required. The transfusion should not restart unless the patient receives a satisfactory clinical review.
- Only one type of blood component should be administered at a time. Administering two different types of blood components concurrently (such as platelets and plasma) is not recommended in routine practice because, in the event of an adverse reaction, it is difficult to ascertain which component was responsible. This may be unavoidable in an emergency situation.
- Start the transfusion as soon as possible after removing the blood component from approved temperature-controlled storage. Transfusion of each pack should be completed prior to the labelled expiry or within four hours, whichever is sooner.
- The infusion should start slowly where clinically appropriate. The patient should be closely observed for the first 15 minutes of the infusion as life-threatening reactions may occur after infusion of only a small volume. After 15 minutes, the rate of infusion may be increased to the maximum prescribed rate, provided there are no signs or symptoms of an adverse reaction.
- Transfusion of each unit may proceed as fast as prescribed and tolerated. The infusion rate for blood components depends on the clinical context, age and cardiac status of the patient. In stable, non-bleeding adult patients, typical administration durations are:
- Red cells 1 - 3 hours
- Platelets 15 - 30 minutes per standard adult dose
- Fresh frozen plasma 30 minutes per unit
- Cryoprecipitate 30 - 60 minutes per standard adult dose
- After completion of the transfusion, blood administration sets may be flushed with 0.9% sodium chloride to ensure that the patient receives all of the blood component. Only the minimum volume of 0.9% sodium chloride required to completely clear the IV line should be used, taking into consideration the individual circumstances of the patient (for example, neonates, some paediatric patients or patients at risk of fluid overload or on fluid restrictions).
For more details on specific aspects of blood component administration, consult the Guidelines for the Administration of Blood Components.
Updated January 2026