Component compatibility
Patients should receive ABO-identical blood products whenever possible, however sometimes it may be necessary to provide ABO-compatible blood products instead.
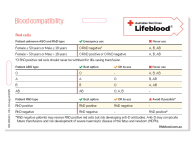
The table below lists the acceptable blood group choices in order of preference.
Red cells
Pretransfusion testing is required to identify compatible red cells. Consult your Transfusion Service Provider about your requirements for samples and request forms.
| Patient unknown ABO and RhD type | Emergency use | Never use |
| Female ≤ 50 years or Male ≤ 18 years | O RhD negative# | A, B, AB |
| Female > 50 years or Male > 18 years | O RhD positive or O RhD negative | A, B, AB |
# O RhD positive red cells should never be withheld for life-saving transfusion.
| Patient ABO type | Best option | OK to use | Never use |
| O | O | - | A, B, AB |
| A | A | O | B, AB |
| B | B | O | A, AB |
| AB | AB | O, A, B | - |
| Patient RhD type | Best option | OK to use | Avoid if possible* |
| RhD positive | RhD positive | RhD negative | - |
| RhD negative | RhD negative | - | RhD positive* |
* RhD negative males (>18 years) and females not of childbearing potential (> 50 years) may safely be given RhD positive red cells but have a risk of developing anti-D antibodies.
The following patient groups should receive RhD negative red cells:
- RhD negative patients with anti-D
- RhD negative females of childbearing potential
- Females of childbearing potential with unknown blood group (in an emergency)
- RhD negative paediatric males, and
- RhD negative patients who will receive repeated transfusions or are likely to become transfusion dependent.
Some regional and smaller metropolitan hospitals may only hold O RhD positive red cells for emergency use (e.g. in life-threatening situations).
Kell blood group system compatibility
Kell blood group system antibodies should be considered clinically significant and are known to cause both transfusion reactions and haemolytic disease of the fetus and newborn (HDFN).
The Australian and New Zealand Society of Blood Transfusion (ANZSBT) and Lifeblood released a joint Consensus statement on use and allocation of Kell negative red cells to assist in the equitable and appropriate availability of K negative red cells.
Clinical scenarios where K negative red cells are indicated (listed in priority order) include:
Any patient with (or a history of) anti-K.
- Transfusion of pregnant females or females of childbearing potential (≤ 50 years) who are K negative (∼90% of women).
- Transfusion of pregnant females or females of childbearing potential who are unable to be phenotyped prior to transfusion. The clinical urgency of transfusion should be considered, and emergency transfusion should not be delayed by attempts to source K negative units.
- Patients receiving daratumumab (anti-CD38 monoclonal antibody) therapy who are K negative or whose K phenotype (or genotype) cannot be determined
- Transfusion-dependent patients who are shown to be K negative (∼90% of patients). However, laboratories may choose the option of transfusing K negative units only if the patient subsequently develops anti-K.
Platelets
| Patient ABO type | Best option | OK to use |
| Unknown (emergency issue) | O* or A* | A, B |
| O | O | A#, B, (A, AB) |
| A | A | B*, O*, (AB) |
| B | B | A*#, O*, (AB) |
| AB | AB (not routinely available) | A*, B*, O* |
Note:
*Low-titre anti-A/B apheresis platelets or pooled platelets pose a lower risk of haemolysis when transfusing ABO incompatible components. Check with the laboratory if unsure.
#Group A platelets with the A2 subgroup have decreased expression of A antigen and are therefore preferable to other group A platelets when transfusing group O and B recipients.
If it’s necessary to provide platelets with a blood group other than the patient’s own, the clinical circumstances, specific component availability (pooled vs apheresis) and a requirement for special components (e.g. HLA or HPA matched), may influence the decision to give platelets that are ABO incompatible with the recipient:
- If transfused platelets have an ABO antibody incompatible with the recipients red cells. (e.g. group A patient receiving group O platelets), the recipient may develop haemolysis and a positive direct antiglobulin test (DAT). This is of greater importance in children as they have lower levels of soluble A and B substance in their body fluids which would otherwise contribute to neutralising the transfused ABO antibodies.
- If transfused platelets are ABO antigen incompatible with recipient’s ABO antibody (e.g. group O patient receiving A platelets), their anti-A and/or Anti-B would result in clearance of donor platelets and the post-transfusion platelet increment (PPI) and platelet survival may be lower than expected.
Platelets do not express Rh antigens but alloimmunisation to RhD may occur due to residual RhD positive red cells in the platelet component. Platelets with the same RhD type as the recipient are the ideal option. If RhD positive platelets are given to an RhD negative female of childbearing potential, RhD immunoglobulin (RhD-Ig) should be given.
RhD immunoglobulin may also be indicated for other RhD negative patients receiving RhD positive platelets.
Plasma
Using group A clinical plasma for emergency blood resuscitation is a safe alternative that provides clinical benefit and eases pressure on group AB donors and supplies.
| Patient ABO blood type | First choice | Second choice | Third choice | Fourth choice |
| O | O | A | B | AB |
| A | A | AB | ||
| B | B | AB or A* (low titre) | ||
| AB | AB | A* (low titre) | ||
Adults and paediatrics Unknown (emergency issue) | A* (low titre) | AB | A | |
Neonates and infants <1 yr old Unknown (emergency issue) | AB or A* (low titre) | A |
* Low titre A/B plasma *poses a lower risk of haemolysis when transfusing ABO incompatible components. Check with the laboratory if unsure.
Plasma components (e.g. fresh frozen plasma, cryoprecipitate and cryodepleted plasma) should be compatible with the ABO group of the recipient to avoid potential haemolysis caused by donor anti-A or anti-B.
If an ABO incompatible plasma transfusion is given (e.g. group B or AB patients receiving group A plasma), the patient may develop haemolysis and a positive direct antiglobulin test (DAT). This is of greater importance in children as they have lower levels of soluble A and B substance in their plasma.
Plasma components of any RhD type can be given regardless to the RhD type of the recipient. RhD immunoglobulin is not required in these situations.
Updated June 2025