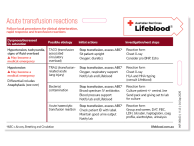
Management of suspected reactions
As soon as you suspect a transfusion reaction:
- Stop the transfusion immediately and activate emergency procedures if required.
- Assess patient’s Airway, Breathing and Circulation (ABC). Check and monitor the patient’s vital signs.
- Maintain intravenous (IV) access (do not flush the existing line and use a new IV line if required).
- Repeat all clerical and identity checks; ensure the right pack has been given to the right patient. Visually inspect the pack for clots, haemolysis, unusual discoloration or cloudiness).
- Notify your Medical Officer and Transfusion Service Provider.
Follow local procedures for clinical deterioration, rapid response, and identification and management of transfusion reactions. After the transfusion has been stopped (except for some types of mild reaction), you may be required by the Transfusion Service Provider to send them freshly collected blood and urine samples along with the used component pack and IV line. Follow your relevant organisational occupational health and safety policies at all times (e.g. do not transport IV lines with the insertion spike (sharp end) exposed).
Document the reaction in the patient’s medical record and complete an incident report if required by local policies.
For further information on the hospital management and investigation of suspected transfusion-transmitted bacterial infection refer to our 'Guidelines for hospital investigation of transfusion related sepsis' and 'Guidelines for the microbiology laboratory processing of blood components associated with transfusion reactions'.
Common adverse transfusion reactions and a guide to appropriate clinical action and investigations
- Fever (>38°C and rise ≥1°C)
>38°C and rise ≥1°C to <1.5 °C from baseline within 4 hours of starting transfusion without other signs/symptoms Possible etiology Action Investigation Mild Febrile non-haemolytic transfusion reaction (FHNTR) STOP transfusion.
Exclude serious adverse events.
Give an anti-pyretic.
Recommence transfusion slowly if the reaction subsides and observe closely.
If no improvement or worsening of symptoms, stop transfusion and do not restart.
Send a reaction form to the laboratory as per local procedure.
Consider unrelated causes of fever.
≥ 39°C or rise ≥1.5°C from baseline OR with other signs/symptoms such as chills/rigors, hypo/hypertension, shock, tachycardia, respiratory distress, localised pain, and nausea/vomiting.
Potentially life-threatening.
Possible etiology Action Investigations Moderate/severe Febrile non-haemolytic transfusion reaction (FHNTR)
OR
Transfusion-transmitted bacterial infection (TTBI)
OR
Acute haemolytic transfusion reaction (AHTR)
May become a medical emergency
STOP transfusion, do not restart.
Moderate to severe febrile non-haemolytic transfusion reaction (FNHTR)
FNHTR is a diagnosis of exclusion.
Investigate for serious reactions with work-ups for sepsis (TTBI), incompatible blood (AHTR) and DIC.
Transfusion-transmitted bacterial infection (TTBI)
Commence broad-spectrum IV antibiotics, maintain BP/urine output (IV fluids, inotropes as needed).
Ask your Transfusion Service Provider to notify Lifeblood to quarantine components from the same donation.
Acute haemolytic transfusion reaction (AHTR)
Maintain BP/urine output (IV fluids, inotropes as needed).
For further transfusions, consult a haematologist.
Send a reaction form to the laboratory as per local procedure.
Sepsis work-up including
Septic screen, including blood cultures on patient +/- central line.
Send pack + giving set to laboratory for culture.
Incompatible blood work-up
If an incorrect pack is given, notify the laboratory immediately.
Group and screen and DAT on pre- and post-transfusion samples.
Haemolysis screen: FBC, LDH, bilirubin, haptoglobin, electrolytes, creatinine, urinalysis.
DIC work-up (may occur in a severe reaction)
aPTT, PT, fibrinogen, D-Dimer.
- Urticaria or rash
Isolated urticaria (hives), pruritus without other signs/symptoms (during or within 4 hours of transfusion)
Potentially life-threatening if progresses.
Possible etiology Action Investigation Minor allergic reactions - rash/pruritus without other features STOP transfusion.
Stop/pause other possible allergens.
Give antihistamine. Assess and monitor for possible progression.
If the reaction subsides and the product is still viable, restart the transfusion slowly and observe closely.
If no improvement or worsening of symptoms, stop the transfusion and do not restart.
If recurrent minor allergic reactions occur, consider premedication with an antihistamine.
No investigation required. Generalised erythema, urticaria, localised angioedema without airway involvement or respiratory compromise or hypotension.
No other signs/symptoms.
Potentially life-threatening if progresses.
Possible etiology Action Investigation Allergic reaction - skin and subcutaneous tissues only without airway involvement STOP transfusion, do not restart.
Stop/pause other possible allergens.
Assess and monitor for possible progression – refer to local anaphylaxis protocol.
Give an antihistamine and a corticosteroid as required.
If recurrent allergic reactions occur, consider premedication with an antihistamine and consultation with a haematologist.
No investigation required. Rapidly developing features of airway, breathing, or circulation (ABC) problems usually with skin and/or mucosal changes
Within 45 minutes of starting transfusion (majority within 5 minutes).
With other sign/symptoms such as:
- Respiratory compromise e.g. stridor, swelling, bronchospasm, dyspnoea, hypoxia.
- Hypotension or end-organ compromise e.g. syncope, incontinence.
- Severe GI symptoms, e.g. vomiting, abdominal pain.
Refer to local anaphylaxis protocol for clinical criteria to support prompt diagnosis; acute onset of hypotension or bronchospasm or laryngeal involvement may occur in absence of typical skin involvement.
Potentially life-threatening if progresses.
Possible etiology Action Investigations Anaphylaxis
(consider IgA deficiency)STOP transfusion, do not restart. Stop/pause other possible allergens.
Treat per local anaphylaxis protocol, including adrenaline, oxygen, and IV fluids.
For further transfusions, consult a haematologist. To prevent recurrence, consider an antihistamine +/- steroid premedication.
If IgA deficient with IgA antibodies, consider washed red cells and IgA deficient components.
Anaphylaxis work-up
Serial tryptase, IgA levels (+ anti-IgA antibodies if IgA deficient) and haptoglobin.
- Dyspnoea, shortness of breath, decreased oxygen saturation
Within 15 minutes of starting transfusion but may be later.
Hypotension, with/without fever, tachycardia.
Potentially life-threatening.
Possible etiology Action Investigation Transfusion-transmitted bacterial infection (TTBI)
OR
Acute haemolytic transfusion reaction (AHTR)
OR
STOP transfusion, do not restart.
Transfusion-transmitted bacterial infection (TTBI)
Broad-spectrum IV antibiotics, maintain BP/urine output (IV fluids, inotropes as needed).
Ask your Transfusion Service Provider to notify Lifeblood to quarantine components from the same donation.
Acute haemolytic transfusion reaction
Maintain BP/urine output (IV fluids, inotropes as needed).
For further transfusions, consult a haematologist.
Anaphylaxis
Stop/pause other possible allergens.
Treat per local anaphylaxis protocol, including adrenaline, oxygen, and IV fluids.
For further transfusions, consult a haematologist. To prevent recurrence, consider an antihistamine +/- steroid premed.
If IgA deficient with IgA antibodies, consider washed red cells and IgA deficient components.
Sepsis work-up
Blood cultures on the patient +/- central line.
Septic screen for other sources.
Send pack + giving set to lab for culture.
Incompatible blood work-up
If an incorrect pack is given, notify the laboratory immediately.
Group and screen and DAT on pre- and post-transfusion samples.
Haemolysis screen: FBC, LDH, bilirubin, haptoglobin, electrolytes, creatinine, urinalysis.
DIC work-up (may occur in a severe reaction)
aPTT, PT, fibrinogen, D-Dimer.
Anaphylaxis work-up
Serial tryptase, IgA (+/- IgA antibodies), haptoglobin.
Others, as per local guidance.
During or up to 12 hours following transfusion (mostly within 1–2 hours)
Typically with hypertension, also hypoxaemia, orthopnea, raised JVP, tachycardia, basal crackles, positive fluid balance.
Potentially life-threatening.
Possible etiology Action Investigation Transfusion associated circulatory overload (TACO) Stop transfusion, do not restart. Pause concurrent IV fluids.
Give oxygen, diuretics and sit the patient upright.
For future transfusions in susceptible patients (e.g. paediatric or elderly patients, severe anaemia, impaired cardiac or renal function): infuse slowly and consider a diuretic.
Assess CXR for acute pulmonary oedema (APO).
Assess other cause(s)/contributors to APO.
Elevated pro-BNP is more common in TACO, consider an echocardiogram.
During or within 6 hours following transfusion (usually within 1–2 hours)
Typically with hypotension, also hypoxaemia, bilateral pulmonary crackles, cyanosis, fever, tachycardia, JVPNE.
No evidence of circulatory overload or pre-existing lung injury.
Potentially life-threatening.
Possible etiology Action Investigation Transfusion-related acute lung injury (TRALI) Stop transfusion, do not restart.
Give oxygen; supportive care and expert evaluation for ventilatory support; diuretics are not beneficial and may worsen TRALI. Consult haematologist.
Ask your Transfusion Service Provider to notify Lifeblood as quarantine and testing components from the same donation may be required.
Assess CXR for bilateral interstitial and alveolar infiltrates.
Normal pro-BNP is more common in TRALI; consider an echocardiogram.
HLA/HNA typing (consult Lifeblood).
Note: TRALI is a clinical diagnosis – investigations to exclude other reactions.
Note that this is a guide only. You must follow your hospital guidelines. Inform Lifeblood of any adverse reaction that may:
- relate to the quality of the product which will prompt Lifeblood to recall any associated products, e.g. transfusion transmissible infections, and TRALI; or
- require an alternative product to be requested e.g. washed red cells in patients with repeated anaphylactic reactions or IgA deficient products.
Clinical management must be tailored to the patient’s specific situation in consultation with the treating Medical Officer, Haematologist or Transfusion Service Provider.
Updated October 2025