Parents' and carers' guide to transfusion
What is a blood transfusion?
A blood transfusion involves blood being given through a tube into the bloodstream.
It is used to replace blood or the part of the blood that has been lost, is missing or not working properly.
The team caring for you child will explain:
- why transfusion is being recommended or might be needed
- other possible options for treatment
- the expected benefits
- the possible risks and side effects
- which blood products will be transfused
- how the transfusion will be given and how long it will take
Which blood product might my child receive?
After Lifeblood collects blood from a donor it is separated into parts, so your child only receives the part that they need. The different parts are stored in special bags or bottles.
- Red blood cells
Red blood cells carry oxygen around the body.
A low number of red blood cells (anaemia) can be due to
too many being lost due to bleeding
too few being made by the body
too many being broken down- Platelets
Platelets are tiny cells in the blood that help to stop bleeding by forming a clot.
A low number of platelets can be due to
too many being used up or lost during bleeding
too few being made
too many being broken up- Plasma (fresh frozen plasma, cryoprecipitate)
Plasma is the liquid part of blood that carries blood cells and different proteins around the body.
These proteins have special jobs such as helping the immune system.
Plasma may be needed to replace the special clotting proteins that are lost during bleeding.- Blood products made from plasma
The different proteins in plasma can be separated to make concentrated versions, stored in glass bottles.
Each type of blood product separated from plasma has a specific purpose:
Albumin helps maintain fluid levels.
Immunoglobulins help the immune system.
Clotting factors are for treating specific bleeding problems.
Frequently asked questions
- Why might my child need a blood transfusion?
- Blood transfusions are used to treat anaemia (lack of red blood cells or poor-quality red blood cells).
- Most people cope well with losing a moderate amount of blood. Over the next few weeks, the body makes new red blood cells to replace those lost.
- Medicines such as iron can help compensate for blood loss. But if larger amounts are lost, a blood transfusion is the best way of replacing the blood quickly.
- Blood transfusions are given to replace blood lost in surgery, and after serious injury or accidents.
- Some operations or medical treatments (including many types of chemotherapy) cannot be carried out safely without using blood products.
- What can be done to reduce my child’s need for blood before an operation?
- Encourage your child to eat a well-balanced diet in the weeks before the operation.
- Your child may need to have their iron levels boosted – ask your child’s doctor for advice especially if you know that your child has suffered from low iron levels in the past.
- If your child is on blood thinning medication, stopping these drugs may reduce the amount of bleeding. Always ask your child’s doctor whether these should stop before the operation and when. (Please remember, for your child’s safety, only his/her doctor can make this decision.)
- Sometimes it is possible to collect blood that is lost during or after an operation and return it back to your child. You may want to ask if this method is possible in your child’s case.
- What would happen without a transfusion?
A transfusion will be given only if medically necessary. For example, red cells carry oxygen and once anaemia becomes severe, your child’s body may not be getting enough oxygen. This could lead to heart, kidney or brain problems. Please talk with your clinical team about any concerns. Ask your child’s doctor to explain why your child needs a transfusion and if there are any alternative treatments available.
- Will this transfusion affect my child in the future?
From what we know so far, there are limited long-term effects. If your child needs a transfusion in the future, remember to mention that they have had one before as it can help choosing the best blood for them.
- Can I donate my blood to my child?
The risks from receiving blood from donors provided by Lifeblood is extremely low, so parents’ blood is not used. In addition, there are some increased risks of rare transfusion reactions when children receive blood from relatives.
- Are transfusions safe?
A blood transfusion is a common and generally safe procedure.
- Lifeblood collects blood for transfusion in Australia from voluntary donors.
- Our blood supply is one of the safest in the world and most children will have no complications during or after their transfusion.
- Although transfusions are generally very safe, there are some associated risks. However, precautions are taken to avoid any complications.
There are three key risks to be aware of:
Having a reaction Reactions are uncommon.
- Mild reactions are the most common and include a rash or slight fever.
- Severe reactions include breathing difficulties, high fever and severe allergy (anaphylaxis).
- Your child will be carefully monitored during and after the transfusion.
- Alert the nursing staff if you have any concerns about your child during the transfusion.
Catching an infection The risk of infection from a transfusion is very low.
- In Australia, blood is carefully screened for infections. This includes screening donors and testing the blood after it has been donated.
- The risk of catching any diseases such as Hepatitis C or HIV is less than one in a million.
- Some blood products (platelets) are also tested for bacteria to reduce the chance they carry any bacteria.
- The needles and blood donation equipment are sterile and only used once.
- The testing process is continuously monitored to make sure that it meets very high standards.
Receiving the wrong blood product This is a rare occurrence and is usually caused by an error in name checking.
- To ensure your child receives the right blood, the laboratory and clinical staff make careful identification checks before any transfusion.
- It is important that your child is wearing an identification (ID) band throughout the process.
- The clinical staff will ask you or your child to state their full name and date of birth.
- They will then check the details on your child’s ID band and blood pack to ensure that your child receives the right blood.
- You can help by making sure this process happens.
How is the blood chosen?
A blood sample is taken before starting the blood transfusion, to check the donor blood pack is the right blood group.
Donated blood will be specially selected to be compatible with your child’s blood.
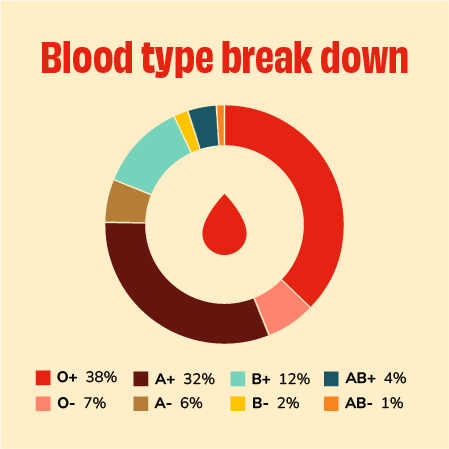
Everyone has a main blood type made up of ABO (so A, B, AB or O) and Rh(D), which is positive or negative. There are eight main blood types.
Along with these eight main blood types, there are also hundreds of sub-blood types. The transfusion will be specially selected to match with your child’s main blood group.
Some people may develop an antibody (a molecule that attacks foreign things in the blood) that means they need blood matched even more closely to their type.
Less than 1 in 20 adult patients develop an antibody to a blood group in the donor blood. This is less common in children but higher in people requiring multiple transfusions.
If you know that your child has special transfusion requirements, please discuss these with your child’s doctor and ask the doctor to tell the hospital transfusion laboratory.
How is blood given?
It is dripped into a vein, usually in your child’s arm or hand, using an intravenous (IV) cannula. An IV cannula is a small, soft plastic tube put directly in your child’s vein using a needle. The link below will take you to a video of a child having an IV cannula inserted.
- The blood product will be carefully checked to make sure it matches your child’s blood.
- One pack of blood (a unit) takes up to 4 hours to give, but can be given slower or faster if it’s needed.
- During this time your child may be able to sit in a reclining chair, play on their phone or iPad, listen to music or watch something. Check with your child’s clinical team what other activities they can do during the transfusion.
- Once it’s finished, if the IV cannula is no longer required, it will be removed.
- A bandage is put over the area, which may be a bit tingly or sore for a little while.
Before you leave hospital, the clinical team will give you information about possible side effects to look out for and who to contact.

Become a blood donor
Many people today would not be alive if it wasn't for generous, volunteer blood donors who give blood regularly to help those in need. It's one of those things that we just expect to be there for us, but only a very small proportion (less than 5%) of people actually give blood. If you would like to help others by becoming a blood donor, please call:
Australia - 13 14 95

