Use of platelets
Indications
Therapeutic platelet transfusions are used for the treatment of bleeding due to thrombocytopenia or functionally abnormal platelets (e.g. inherited platelet disorder).
Prophylactic platelet transfusions are used to prevent bleeding in patients with thrombocytopenia or functionally abnormal platelets (e.g. secondary to cancer or chemotherapy).
The decision to transfuse platelets should take into account the patient's clinical status, the potential risks and benefits, and not dictated by platelet count alone.
Refer to the National Blood Authority's Patient Blood Management Guidelines and other evidence-based clinical guidelines for specific guidance to support clinical decisions about appropriate transfusion practices and the use of blood components.
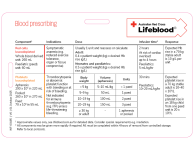
Our Prescribing platelets table provide guidance for transfusion based on the patient's condition and platelet count. It’s based on the above guidelines.
Phrophylactic platelet transfusion for prevention of bleeding
| Acceptable indications | Platelet threshold |
|---|---|
| Neurosurgery | <100 x 109/L |
| Invasive procedures | <50 x 109/L |
| Vaginal or caesarean birth | <50 x 109/L |
| Central venous catheter (CVC) insertion (elective) | <20 x 109/L |
| Critically ill patients | <20 x 109/L |
| Chemotherapy or haematopoietic stem cell therapy (HSCT) with risk factors [a] | <20 x 109/L |
| Chemotherapy or haematopoietic stem cell therapy (HSCT) without risk factors | <10 x 109/L |
| Preterm and low birthweight infants | <25 x 109/L |
| Preterm neonate with FNAIT [b] | <50 x 109/L |
| Term neonate with FNAIT [b] | <30 x 109/L |
| All other patients | <10 x 109 /L |
[a] Risk factors: fever, minor bleeding, sepsis.
[b] Paediatric haematologist should be consulted.
Therapeutic platelet transfusion
| Acceptable indications | Platelet threshold |
|---|---|
| Thrombocytopenia with clinically significant bleeding [a] | <30 x 109/L |
| Thrombocytopenia with severe bleeding [b] | <50 x 109/L |
| Thrombocytopenia with bleeding at critical sites [c] | ≤100 x 109/L |
| Congenital or acquired functional platelet defects | Platelet counts are not a reliable indicator |
| Disseminated Intravascular Coagulopathy (DIC) | Aim for >50 x 109/L |
| Immune thrombocytopenia (ITP), Thrombotic thrombocytopenia purpura (TTP), Heparin-induced thrombocytopenia (HIT) | <20 x 109/L (only if bleeding) |
| Fetal and Neonatal Alloimmune Thrombocytopenia (FNAIT) with intracranial bleeding | <100 x 109/L |
| Fetal and Neonatal Alloimmune Thrombocytopenia (FNAIT) with other bleeding | <50 x 109/L |
[a] Clinically significant bleeding e.g. prolonged epistaxis, extensive skin bleeding, haematemesis, melaena, WHO grade 2.
[b] Severe bleeding e.g. bleeding that requires a RBC transfusion, WHO grade 3-4.
[c] Critical sites e.g. CNS, eyes.
When are platelets not indicated?
Platelets should not be used:
- in bleeding unrelated to thrombocytopenia or abnormally functioning platelets
- in patients with immune mediated thrombocytopenia such as in immune thrombocytopenic purpura (ITP), thrombotic thrombocytopenic purpura (TTP), or heparin-induced thrombocytopenia (HIT), unless the patient has life-threatening haemorrhage, and
- prophylactically following cardiac surgery.
Dosage
The usual dose for an adult patient is 1 unit of apheresis platelets or 1 pooled platelet unit.
One unit apheresis or pooled leucocyte depleted platelets would be expected to increase the platelet count of a 70 kg adult by 20–40 x 109/L.
The suggested dose of platelets for transfusion in neonates and infants is 10 mL/kg.
One unit of paediatric apheresis leucocyte depleted platelets would be expected to increase the platelet count of an 18 kg child by 20 x 109/L.
Do not routinely transfuse more than a single dose of platelets. Reassess patient’s clinical condition and consider checking the post-transfusion platelet count after transfusion.
Updated May 2025