Use of red cells
Indications
Red cells are used for the treatment of clinically significant anaemia with symptomatic deficit of oxygen carrying capacity.
Decision to transfuse should not be dictated by a haemoglobin 'trigger' alone, but should be based on assessment of the patient’s clinical status and individual patient factors including:
- The clinical signs and symptoms fo anaemia.
- The cause for anaemia and if alternative therapies are available (e.g. iron therapy).
- The patient's underlying condition and comorbidities.
- Balancing the evidence for efficacy and improved clinical outcome against the potential risk, and
- The response to previous transfusions.
In haemodynamically stable patients, many studies and guidelines support the use of restrictive transfusion practice. When using a restrictive Hb threshold consider transfusing when Hb is below 70 g/L.
However a restrictive transfusion strategy does not apply to a subgroup of patients including patients with acute coronary syndrome and patients who are transfusion dependent with chronic anaemia (e.g. sickle cell disease, thalassaemia and myelodysplastic syndrome).
In patients with acute coronary syndrome, consider setting a higher transfusion threshold i.e. Hb < 80 g/L. Decision around appropriate Hb threshold and frequency of transfusion for patients who are regularly and chronically transfused should be individualised and guided by patient's anaemia-related symptoms, functional status, and response to previous transfusion.
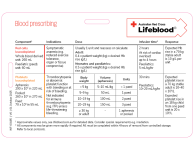
Our prescribing red cells table provides guidance for transfusion based on the patient’s condition and haemoglobin level. It’s based on the National Blood Authority’s Patient Blood Management Guidelines.
Refer to the National Blood Authority Patient Blood Management Guidelines and other evidence-based clinical guidelines for specific guidance to support clinical decisions about appropriate transfusion practices and the use of blood components.
When should red cell transfusion be avoided?
The transfusion of red cells is not recommended for the treatment of anaemia associated with iron, vitamin B12 or folate deficiency if the patient’s clinical condition permits sufficient time for erythropoiesis following replacement. See Iron deficiency anaemia for more information.
Modifications
Red cells can be modified for specific indications and patient groups.
Dosage
The transfusion of a unit of red cells is expected to increase the haemoglobin of a 70 kg non-bleeding patient by approximately 10 g/L.
For haemodynamically stable inpatients, transfusion of a single unit of red cells followed by clinical reassessment to determine the need for further transfusion is considered best practice. A post-transfusion haemoglobin check is not mandatory but may be useful in some clinical situations.
Whenever possible, transfuse ABO and RhD group identical red cells. In an emergency situation when the patient’s blood group is unknown, Group O red cells must only be used. RhD status of the group O red cells should be determined by patient factors, see more on use of Group O RhD negative red cells. A blood sample should be taken for blood grouping prior to commencing transfusion to determine the patient’s blood group should ongoing transfusions be required.
Updated May 2025