Don’t have an account?
Select the donation type you’d like to make
Research study update: Beyond the iron gate
Take Home Message
People with Hereditary haemochromatosis (HHC) who donate at Lifeblood reported that they feel more like donors than patients. This suggests that Lifeblood could change the way we communicate with them, as we currently communicate with them as “patients”. They did not know much about plasma and had mixed views on being able to donate plasma.
What was the question?
We wanted to understand the views of people with hereditary Haemochromatosis (HHC) who undergo therapeutic venesection at Lifeblood. We wanted to explore whether they identify as donors, their experiences of donating at Lifeblood, what they knew about their condition, and their knowledge about plasma and whether they would be open to donating other products.
Why is it important?
Lifeblood collects over 36, 000 whole blood donations a year from its growing HHC donor panel consisting of approximately 18 000 donors. It’s important that Lifeblood understands the specific needs of these donors to make their experience a positive one and support their donation schedules. Lifeblood has also considered expanding eligibility of plasma donation to HHC donors, in order to facilitate this expansion we wanted to understand these donors experiences of donating blood, identify any opportunities for improvement, and find out their views on donating plasma.
What did we do?
- We interviewed 15 donors and asked them about living with HHC and donating at Lifeblood.
- We used this information to create a survey.
- The survey was sent to all therapeutic donors who have donated in the last 5 years (18,000 HHC donors).
- We received survey responses from 4,354 (24%) therapeutic donors.
What did we find out?
Identification as a blood donor
Surveyed donors reported strongly identifying as blood donors (Med: 6, scale 1 (Not at all)- 7 (Very much)). Interview participants provided a varied response, explaining that they associated ‘donation’ with giving blood for others. Some considered themselves to be donors because their blood was being used, while others indicated they were donating for their own health and likely would not donate without their diagnosis. A donor who was a previous volunteer donor reported their focus had switched to a more health focused reason:
"I understand I’m doing it fundamentally for my own good. But I’m quite happy that at least it’s – it has the potential to do good things for other people"
Compliance with their treatment regime.
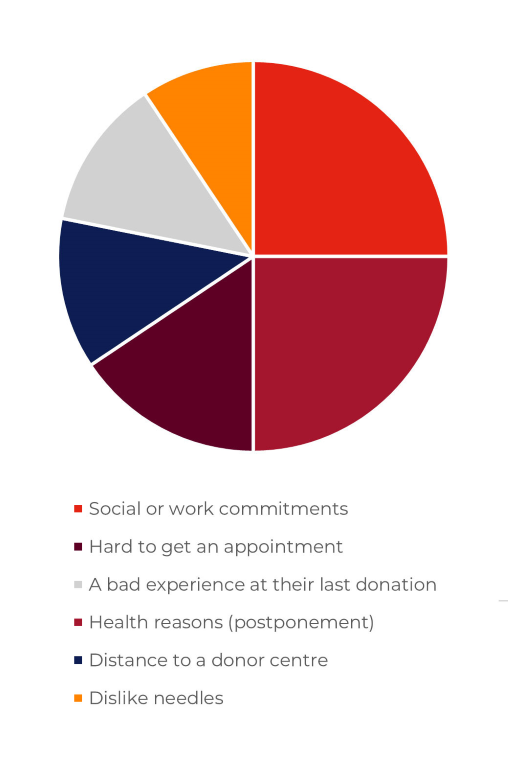
Surveyed donors reported a high compliance to their venesection schedule. When asked for reasons why they would miss an appointment the main reasons were social or work commitments (8%), health reasons that would result in a postponement (8%), hard to get an appointment (5%), the distance to the donor centre (4%), a bad experience at their last donation (4%) and a dislike of needles (3%).
Donating at Lifeblood
62% of surveyed donors came to Lifeblood becasue they know their blood is used and 90% reported this as an enabler. Other enablers were easy access to donor centres (72%), ease of managing their condition (58%), customer service (47%) and phlebotomy skills (45%).
The barriers to donating at Lifeblood, were not being able to manage their own appointments (23%), repeated questioning (18%), donation being postponed (13%) and difficult veins (13%).
Knowledge about blood and plasma
Most donors surveyed knew their blood was being used (62%) but about half were not sure what it was used for. Lifeblood staff were identified as the primary source of providing this information.
Overall, participants reported not having a large amount of knowledge about plasma donation. Those interviewed reported having a general awareness through observation in centre or word of mouth
"Oh well, when you go there, you see people donating the plasma. So you see there’s two different processes"
When asked about interest, those surveyed reported a mixed response with some very interested and others not interested at all (range 1 Not at all interested- 7 Very much). When asked why they wouldn’t be interested the main reason being concerns around their vein health, more needles and length of donation. For those interested the main reasons were helping others and benefit to the community. Those interviewed provided similar reasons but required more information about the benefits and processes prior to deciding.
What are the next steps?
We’ll use the findings from work to improve the experiences of our therapeutic donors.
If you’d like more information about this study, please contact Elizabeth Knight (eliknight@redcrossblood.org.au)
Thank you to all the donors who completed the survey or were involved in phone interviews.






