Don’t have an account?
Select the donation type you’d like to make
Nervous, relaxed, proud: Understanding novice donors’ feelings
Take home message
Most donors feel nervous before their donation to when the needle goes in, but this changes to relaxed, happy, and proud when they’ve finished. Donors identified strategies they use to manage their emotions and made suggestions about how we can provide more support to novice donors.
What was the question?
What emotions do novice donors feel before, during, and after their donation, and why? What can we do to better support them?
Why is it important?
Emotions play an important role in motivating donation, but they can also stop people from donating. Understanding how donors feel before, during, and after a donation can help us better support them.
What did we do?
We interviewed 11 relatively new donors (1-3 donations) either in a focus group or one-on-one. There was a mix of people who had felt faint or fainted, known as a vasovagal reaction (VVR) or only had uncomplicated donations.
What did we find out?
Many donors felt nervous before their first donation because they didn’t know what to expect or they were worried about feeling faint, needle-related pain, potentially having an unknown health condition, or experiencing a lack of control during their donation. While most donors felt comfortable to let the team know that they’re nervous, a few did not. They managed their feelings by texting with a loved one, looking up information about the procedure and possible adverse events, and talking to staff.
“I liked to know that they thought about everything, like potential side effects or potential issues, and it was all written down. I think that made me more at ease.”
Donors felt trust and relaxed during their donation because of the thorough interview process, perceived competence of the team performing the phlebotomy, and good relationships with the team. They also felt the openness and calm environment helped them feel more relaxed.
“A nurse explained to me what was going to happen. She was absolutely brilliant. She didn’t make me feel rushed. I felt very comfortable.”
After finishing their donation, most donors felt happy and proud. This was reinforced when they read the post-donation SMS telling them that their blood has been used. While donors who had a VVR also experienced disappointment and embarrassment, the care given to them and normalising the experience helped them overcome these emotions.
“The nurse stayed with me the whole time, and just chatted to me and that sort of thing. So that built trust in me, that they just treated it like it was not a big deal.”
Donor recommendations included longer appointment times, virtual donor centre tours, personal testimonies, sharing (a summary of) the donor questionnaire, low sensory hours, more explanation around questions and how we manage VVRs, using the term “nervous” rather than “fear”, and finding an easy way to identify nervous donors.
What are the next steps?
The participants gave us great insights into ways we can improve how we support nervous donors from giving more information before the appointment to providing more support during the donation.
We’re now looking at how collection teams currently support nervous donors. This will help us to develop a tool for teams to help them identify and manage nervous donors.
If you’d like more information about this study or a copy of the full report, please contact Amanda Thijsen (athijsen@redcrossblood.org.au) or Kristen Baker ( krbaker@redcrossblood.org.au).
We would like to thank all the donors who participated in our study.
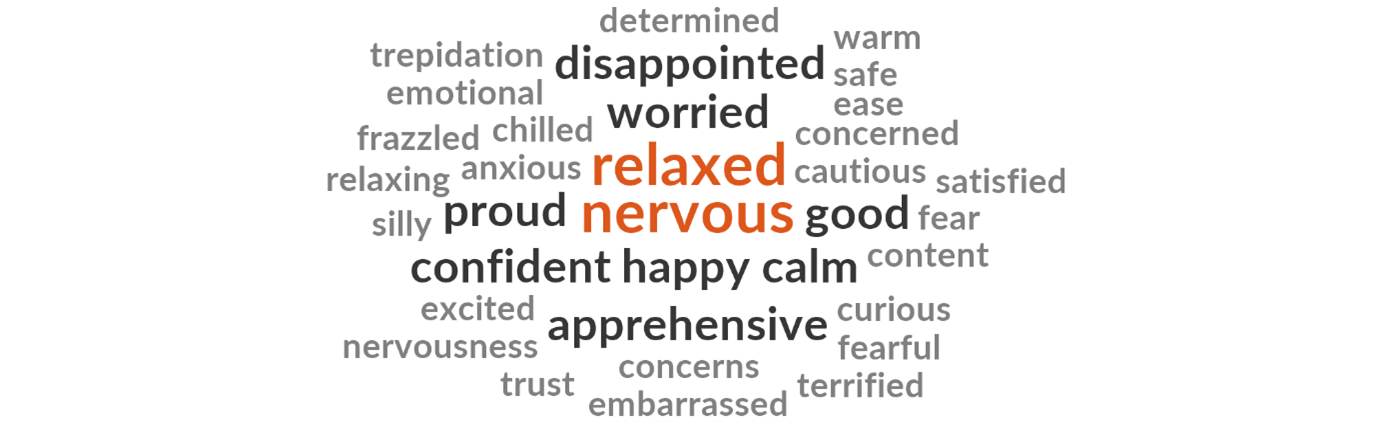
Fig 1: A word cloud describing the emotions experienced by novice donors


