Warfarin reversal
Anticoagulation with Warfarin
Warfarin is a widely used oral anticoagulant for the prevention and management of thromboembolism.
Warfarin works by blocking the gamma-carboxylation of glutamic acid residues of the Vitamin K−dependent coagulation factors II, VII, IX and X.
This inhibition results in the decreased biological activity of factors II, VII, IX, X, and protein C and protein S, causing the prolongation of the international normalised ratio (INR).
Bleeding is the most common complication of Warfarin use, with an annual incidence of warfarin-associated major bleeding of 1%-3%.
The direct oral anticoagulants (DOAC) provide alternatives to warfarin for managing thromboembolic disease in certain patient populations.
Management of an elevated INR caused by warfarin therapy
When considering how to manage patients receiving warfarin who require surgery, the risk of thrombosis if warfarin is withheld needs to be balanced with the risk of bleeding if continued.
The NBA Patient Blood Management (PBM) Guidelines: Module 2 – Perioperative provide some guidance with the following recommendation and practice point.
Recommendation 10:
In patients undergoing minor dental procedures, arthrocentesis, cataract surgery, upper gastrointestinal endoscopy without biopsy or colonoscopy without biopsy, warfarin may be continued (Grade B).
Practice point 10:
In patients receiving warfarin who are scheduled for elective non-cardiac surgery or other invasive procedures (excluding minor procedures—see Recommendation 10); specific management according to current guidelines is required (e.g. guidelines from the American College of Chest Physicians and the Thrombosis and Haemostasis Society of Australia and New Zealand (THANZ).
Major bleeding or urgent surgery are commonly encountered and require prompt reversal of warfarin anticoagulation to counteract the prolonged inhibition of vitamin K-dependent factors. The standard management for urgent warfarin reversal has been vitamin K and Prothrombinex®-VF (3-factor prothrombin complex concentrate; 3-factor PCC) and, if necessary, FFP to provide factor VII. However, the supply of Prothrombinex®-VF was replaced by Beriplex® (4-factor PCC) in June 2024 as part of Australia’s transition to new domestic fractionated products. Beriplex® contains all the vitamin K-dependent coagulation factors (factors II, VII, IX, and X).
Vitamin K alone has been shown to be effective in warfarin reversal but its full effect typically takes 12–24 hours. Where rapid reversal of INR is required (ie, emergency surgery, major bleeding), the use of 4-factor PCC is recommended.
When Beriplex® is used in life-threatening warfarin-related bleeding (in conjunction with IV Vitamin K), FFP is not required for reversal of the warfarin effect as Beriplex® contains sufficient amounts of all 4 of the vitamin K-dependent coagulation factors. FFP may however, be required for associated major haemorrhage as directed by the local Major Haemorrhage Protocols.
THANZ has produced updated recommendations for warfarin reversal in the setting of four-factor prothrombin complex concentrate. All dosing decisions should consider the individual patient, including:
• their degree of bleeding
• the ability to perform timely and adequate haemostatic interventions and
• their underlying thrombotic risk that warranted anticoagulation with warfarin in the first place
In patients > 100 kg, the dose of 4-factor PCC should be calculated based on a capped 100 kg body weight and maximum dose of 50 IU/kg (i.e. maximum dose of 5000 IU).
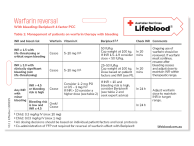
A. Management of patients on warfarin therapy WITH bleeding
- A1: INR ≥ 1.5 with life-threatening or critical organ bleeding
Warfarin Cease Vitamin K Give 5 - 10 mg IV Beriplex® Give 50 IU/kg*
Cap weight at 100 kg
Measure INR In 20 minutes Comments Resume warfarin when bleeding ceases and adjust the dose to maintain INR within the target therapeutic range
* Note: Consider giving a Beriplex® dose < 50 IU/kg when INR 1.5 - 1.9- A2: INR ≥ 2.0 with clinically significant bleeding (not life-threatening)
Warfarin Cease Vitamin K Give 5 – 10 mg IV Beriplex® Give 25 - 50 IU/kg
Cap weight at 100 kg
Dose based on INR (see PI) and patient-level factors (e.g. type of bleeding, need and ability to undergo intervention)
Measure INR In 20 minutes Comments Resume warfarin when bleeding ceases and adjust the dose to maintain INR within the target therapeutic range - A3: Any INR with minor bleeding
Warfarin Omit/Cease Measure INR Within 24 hours Comments Adjust warfarin dose to maintain INR in the target therapeutic range
If bleeding risk is high# or INR > 4.5
- consider vitamin K (1 - 2 mg oral or 0.5 – 1 mg IV)If bleeding risk is high# and INR >10
- consider a higher dose of vitamin K (see B5: INR >10 and bleeding risk is high)
- consider Beriplex® (see B5: INR >10 and bleeding risk is high and seek expert advice)# Note: High bleeding risk: Recent major bleed (within previous 4 weeks) or major surgery (within previous 2 weeks), thrombocytopenia (platelet count, < 50 x 109/L), known liver disease or concurrent antiplatelet therapy
B. Warfarin reversal in patients WITHOUT bleeding
Warfarin cessation before surgery needs to balance the thrombotic risk if warfarin is temporarily stopped against the risk of bleeding related to the ongoing anticoagulation. For patients on warfarin, the periprocedural bleeding risk can be significant, occurring in up to nearly 25% of cases.
The updated 2024 THANZ recommendations for warfarin reversal in the setting of four-factor prothrombin complex concentrate advise that the management of non-bleeding patients on warfarin remain unchanged (from the 2013 update of consensus guidelines for warfarin reversal).
In elective surgery, either omission of warfarin alone or with co-administration of vitamin K is the recommended pathway for warfarin reversal.
Outside of the peri-operative setting, Beriplex® should only be considered if INR > 10, and there is a high risk of bleeding.
- B1: INR higher than therapeutic range but < 4.5
Warfarin Reduce or omit the next dose* Comments Resume warfarin at a reduced dose when INR approaches the target therapeutic range *Note: Dose reduction may not be necessary if the INR is only minimally above therapeutic range (up to 10%) - B2: INR 4.5 – 10 and bleeding risk is low
Warfarin Cease Measure INR Within 24 hours Comments Resume warfarin at a reduced dose when INR approaches the target therapeutic range - B3: INR 4.5 – 10 and bleeding risk is high#
Warfarin Cease Vitamin K Give 1− 2 mg oral or 0.5 – 1 mg IV Measure INR Within 24 hours Comments Resume warfarin at a reduced dose when INR approaches the target therapeutic range # Note: High bleeding risk: Recent major bleed (within previous 4 weeks) or major surgery (within previous 2 weeks), thrombocytopenia (platelet count, < 50 x 109/L), known liver disease or concurrent antiplatelet therapy - B4: INR >10 and bleeding risk is low
Warfarin Cease Vitamin K Give 3 −5 mg oral or IV Measure INR Within 12 hours – 24 hours Comments Resume warfarin at a reduced dose when INR approaches the target therapeutic range - B5: INR >10 and bleeding risk is high#
Warfarin Cease Vitamin K Give 3 − 5 mg oral or IV Beriplex® Consider 15 – 30 IU/kg Cap weight at 100 kg Measure INR Within 12 hours – 24 hours Comments Resume warfarin at a reduced dose when INR approaches the target therapeutic range # Note: High bleeding risk: Recent major bleed (within previous 4 weeks) or major surgery (within previous 2 weeks), thrombocytopenia (platelet count, < 50 x 109/L), known liver disease or concurrent antiplatelet therapy
C. Suggested Beriplex® dose for urgent warfarin reversal in a non-bleeding patient (e.g. before surgery) *
Cap weight at 100 kg
| Initial international normalised ratio (INR) | ||||
| Target INR | 1.5 - 2.5 | 2.6 - 3.5 | 3.6 - 10.0 | > 10.0 |
| 0.9 - 1.3 | 30 IU/kg | 35 IU/kg | 50 IU/kg | 50 IU/kg |
| 1.4 - 2.0 | 15 IU/kg | 25 IU/kg | 30 IU/kg | 40 IU/kg |
Note: * Outside of the peri-operative setting, Beriplex should only be considered if INR > 10 and there is a high risk of bleeding (see B5: INR >10 and bleeding risk is high)
Further information
Robinson D, McFadyen J, Merriman E, Wee TC, Baker R, Tran H. Updated recommendations for warfarin reversal in the setting of four-factor prothrombin complex concentrate. Medical Journal of Australia. https://doi.org/10.5694/mja2.52538